人工关节置换术是治疗终末期关节损伤如骨关节炎、股骨头坏死等疾病的首选手术方法,能够有效缓解患者的临床症状并改善其生活质量。然而,一旦出现关节假体周围感染(periprosthetic joint infection,PJI),则可能给患者带来灾难性的影响。研究表明,尽管髋膝关节的PJI发生率相对较低,为1%~2%[1-2],但随着社会老龄化的发展趋势,接受人工关节置换术的患者数量逐渐增加,PJI已成为术后最严重的并发症之一。PJI具有较高的致残风险,患者往往须进行二次手术并长期使用抗生素,从而增加了个人经济负担和社会医疗保险压力。值得关注的是,目前PJI治疗仍存在较高的失败率:保留假体清创术后失败率为30%~50%[3];关节翻修术后感染复发率高达10%~20%[4-5]。因此,在PJI诊疗过程中,病原学的精确诊断尤为关键。既往研究显示,PJI病原菌主要以葡萄球菌为主,金黄色葡萄球菌(Staphylococcus aureus)占23%~27%[6-8],其致病性与多种毒力因子密切相关;其还能形成生物膜,导致慢性及持续性感染[9]。近年来,小菌落变异体(small colony variant,SCV)日益受到关注。SCV是一种营养缺陷型细菌亚群,是细菌为适应环境所呈现的特殊表型,具有菌落细小、生长迟缓、代谢能力较低及胞内寄生等特点。研究表明,金黄色葡萄球菌小菌落变异体(Staphylococcus aureus small colony variant,SASCV)与人体植入物相关感染(implant-associated infection,IAI)关系密切[10-11]。因其在假体表面的黏附性增强[12],SASCV所致PJI的抗感染治疗效果劣于正常表型(normal phenotype, NP)菌株[11-13],更易转为慢性感染且复发率更高[14]。目前,国内对此类感染中SASCV的分子病原学报道较少。因此,本研究对从北京积水潭医院PJI患者关节液中分离的SASCV进行全基因组测序(whole genome sequencing,WGS),分析其毒力基因、耐药基因及分子分型情况,旨在为进一步探讨SASCV在PJI中的致病机制提供基础数据。
1 材料与方法 1.1 菌株来源及患者资料本研究所用菌株分离自2017年1月—2022年1月北京积水潭医院矫形骨科收治的髋膝关节PJI患者关节液标本。当2份及以上标本中培养出同种细菌时,将其视为病原菌。对19例患者的病历资料进行回顾性分析,其中男性12例,女性7例,年龄55±13岁。均符合肌肉骨骼感染学会(Musculoskeletal Infection Society,MSIS)的PJI诊断标准[15],其中髋关节PJI共5例,膝关节PJI共14例。所有SASCV均为非重复菌株;若同一患者多次分离出相同菌株,则选取首次分离的菌株。参考菌株为金黄色葡萄球菌ATCC 25923。
1.2 菌株分离培养与鉴定将PJI患者关节穿刺液注入血培养瓶(美国BD公司),置于BACTEC FX100体液血液培养仪(美国BD公司)中培养。培养仪报阳性结果后,从血培养瓶中抽取1 mL培养液,接种于哥伦比亚血琼脂平皿(中国郑州安图公司),置于35 ℃微生物培养箱内培养,分别于24 h及48 h观察菌落形态。挑取菌落直径远小于正常菌落(直径约为金黄色葡萄球菌ATCC 25923的1/10;见图 1)或大小明显不一的菌株,再次分离纯化培养后,使用基质辅助激光解吸电离飞行时间质谱(matrix-assisted laser desorption/ionization time-of-flight mass spectrometry,MALDI-TOF MS)仪(德国Bruker公司) 鉴定为金黄色葡萄球菌,将菌株置于-80 ℃冰箱保存。
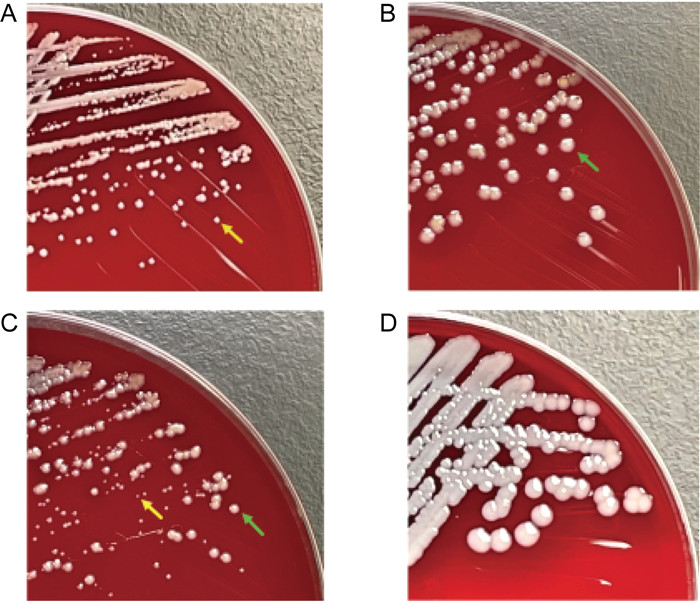
|
| A: Staphylococcus aureus small colony variant (SASCV). B: Staphylococcus aureus normal colony (NP). C: Mixed growth of SCV and NP colonies. D: Staphylococcus aureus ATCC 25923. The yellow arrows point to a SCV colony, and the green arrow points to a NP colony. 图 1 金黄色葡萄球菌小菌落变异体及正常形态(35 ℃,培养48 h) Fig. 1 Staphylococcus aureus small colony variants and normal morphology (35 ℃, after 48 h of incubation) |
将实验菌株接种于哥伦比亚血琼脂平皿(中国郑州安图公司),35 ℃培养48 h后挑取单个菌落,接种于10 mL胰蛋白胨大豆肉汤(trypticase soy broth,TSB)培养液,在35 ℃ 150 r/min条件下振荡培养24 h,10 000 r/min离心5 min,弃上清液后得到菌体沉淀。采用TIANamp DNA提取试剂盒(中国天根生化科技有限公司),按试剂说明书操作提取收集DNA。采用Qubit 4荧光定量仪(美国Thermo Fisher公司)定量,将符合标准的DNA(OD260/280为1.8~2.0,DNA总量≥1 μg,浓度≥20 ng/μL)置于-80 ℃冰箱中保存,用于后续建库与测序。
1.3.2 文库构建及测序将菌株DNA送上海美吉生物医药科技有限公司完成测序:取至少1 μg基因组DNA,利用Covaris超声波打断仪进行DNA片段化,NEXTflexTM Rapid DNA-Seq试剂盒(美国Bio Scientific公司)进行文库制备,Illumina HiSeq X Ten仪器进行双端测序,通过Fastp软件(https://github.com/OpenGene/fastp)对原始测序数据进行剪切,采用SOAP denovo2软件(http://soap.genomics.org.cn)进行拼接,并利用BLASTP、Diamond、Swiss-Prot Database等进行基因功能预测与注释。
1.4 多位点序列分型(multilocus sequence typing,MLST)及系统发育树构建将测序结果与数据库(http://www.mlst.net)比对,获取金黄色葡萄球菌7个管家基因(arcC、aroE、glpF、gmk、pta、tpi、yqiL)的等位基因编码,通过数据库(https://pubmlst.org)比对确定序列分型(sequence type,ST),将至少包含2个ST定义为克隆复合物(clonal complex,CC)分型。使用MEGA 8.0软件针对菌株核心基因序列构建系统发育树,采用Neighbor-Joining法,自展值设为1 000,选取已知金黄色葡萄球菌DSM 20231、头状葡萄球菌NCTC 11045作为参考序列。
1.5 毒力基因与耐药基因注释将测序序列与病原菌毒力因子数据库(virulence factors of pathogenic bacteria,VFDB)比对,进行毒力因子相关基因注释并统计;与耐药基因数据库(https://card.mcmaster.ca和https://cge.cbs.dtu.dk)比对,进行抗生素耐药基因注释并统计。
2 结果 2.1 SASCV的鉴定通过菌落形态筛选及MALDI-TOF MS鉴定,本研究获得19株SASCV,其中8例患者标本中的SCV与NP菌落混合生长(见图 1C)。将8组分离自同一患者的NP和SCV菌落分别标记为sau05-NP/sau05-SCV、sau09-NP/sau09-SCV、sau13-NP/sau13-SCV、sau14-NP/sau14-SCV、sau20-NP/sau20-SCV、sau41-NP/sau41-SCV、sau57-NP/sau57-SCV、sau79-NP/sau79-SCV,纯化培养后用于后续分析。
2.2 菌株全基因组基本特征对19株SCV和8株NP(共27株)进行测序,所得基因组长度为2 696 437~3 011 803 bp,G+C含量为(32.8±0.05)%,测序深度为473±76.6,每个基因组中Contig数量为74.9±28.3个,Scaffold数量为50.7±19.8个,基因数为2 597±99.7个(见表 1)。
| Strain No. | Contig count | Scaffold count | Gene count | Length (bp) | G+C(%) |
| sau05-NP | 67 | 43 | 2 570 | 2 752 741 | 32.83 |
| sau05-SCV | 69 | 43 | 2 574 | 2 755 259 | 32.83 |
| sau09-NP | 43 | 27 | 2 570 | 2 764 016 | 32.69 |
| sau09-SCV | 43 | 28 | 2 573 | 2 762 112 | 32.68 |
| sau13-NP | 67 | 43 | 2 576 | 2 754 681 | 32.83 |
| sau13-SCV | 63 | 40 | 2 570 | 2 748 692 | 32.83 |
| sau14-NP | 42 | 32 | 2 545 | 2 734 647 | 32.75 |
| sau14-SCV | 42 | 29 | 2 547 | 2 737 175 | 32.75 |
| sau20-SCV | 75 | 49 | 2 512 | 2 710 723 | 32.72 |
| sau20-NP | 85 | 57 | 2 515 | 2 724 160 | 32.77 |
| sau27 | 98 | 64 | 2 502 | 2 704 599 | 32.78 |
| sau32 | 90 | 59 | 2 529 | 2 730 817 | 32.74 |
| sau38 | 89 | 65 | 2 703 | 2 858 377 | 32.81 |
| sau39 | 53 | 37 | 2 610 | 2 784 215 | 32.73 |
| sau41-NP | 135 | 90 | 2 939 | 3 011 803 | 32.81 |
| sau41-SCV | 54 | 36 | 2 492 | 2 696 437 | 32.67 |
| sau44 | 85 | 60 | 2 701 | 2 860 531 | 32.81 |
| sau47 | 49 | 34 | 2 619 | 2 784 660 | 32.67 |
| sau56 | 79 | 52 | 2 531 | 2 734 778 | 32.72 |
| sau57-NP | 97 | 73 | 2 741 | 2 866 402 | 32.79 |
| sau57-SCV | 148 | 99 | 2 728 | 2 843 027 | 32.69 |
| sau74 | 108 | 74 | 2 583 | 2 742 964 | 32.73 |
| sau77 | 97 | 69 | 2 617 | 2 794 664 | 32.76 |
| sau79-SCV | 40 | 26 | 2 505 | 2 712 652 | 32.65 |
| sau79-NP | 41 | 26 | 2 500 | 2 713 846 | 32.67 |
| sau80 | 89 | 66 | 2 578 | 2 773 107 | 32.75 |
| sau94 | 74 | 49 | 2 697 | 2 851 598 | 32.74 |
MLST结果显示,19株SCV和8株NP共分10个ST,主要型别为ST59、ST398和ST25,均各检出5株,各占18.5%(5/27);ST22、ST5、ST3687、ST965各检出2株,各占7.4%(2/27);其余ST30、ST188、ST239也有检出,分别占7.4%(2/27)、3.7%(1/27)、3.7%(1/27)。聚类分析显示,10个ST共分为1个CC型和7个单一型(singleton):ST5、ST3687、ST965均属于CC5,在系统发育树上进化关系较密切,其余ST均为单一型(见图 2)。SCV和NP混合生长的菌株中,6组处于系统进化发育树的同一分支(图 2中标识为绿色圆点);其余2组(sau41-SCV/sau41-NP和sau20-SCV/sau20-NP)处于不同分支(图 2中标识为红色三角),菌株为不同ST,且携带的毒力基因及耐药基因不同。sau20-SCV属ST22,mecA基因阴性,而sau20-NP属ST59,mecA基因阳性;sau41-SCV属ST398,mecA基因阴性,而sau41-NP属ST239,mecA基因阳性。各菌株之间的亲缘关系、ST、分离时间,以及mecA、PVL基因检出情况具体如图 2所示。
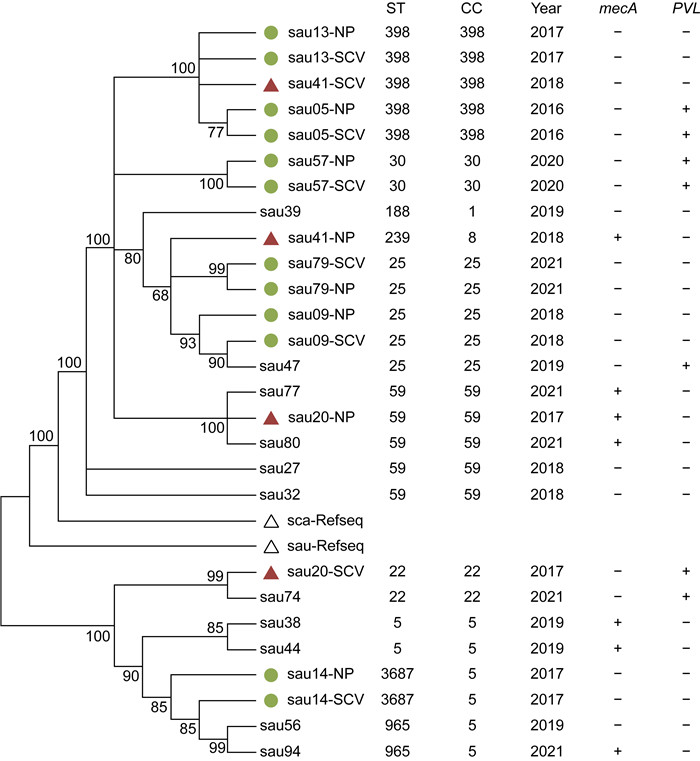
|
| Green dots represent SCV and NP strains isolated from the same patient. Red triangles represent SCV and NP strains isolated from the same patient, with distant evolutionary relationships and different molecular types. 图 2 菌株进化关系树、分子型别及mecA、PVL检出情况 Fig. 2 Phylogenetic tree, molecular type and detection of mecA and PVL |
基于全基因组序列与数据库分析,本研究对金黄色葡萄球菌主要毒力基因进行了比对。在19株SCV中,14种黏附素相关基因的检出率普遍较高。如图 3所示,与生物膜形成相关的icaA、icaB、icaC、icaD和icaR的检出率均超过80%,分别为94.7%(18/19)、100.0%(19/19)、84.2%(16/19)、89.5%(17/19)和84.2%(16/19)。与细胞聚集黏附相关的clfA、clfB、fnbA和fnbB基因检出率分别为89.5%(17/19)、84.2%(16/19)、57.9%(11/19)和73.7%(14/19)。此外,ebh的检出率为100.0%(19/19),ebp为68.4%(13/19),efb为78.9%(15/19),eap/map为78.9%(15/19),而cna为21.1%(4/19)。与细菌免疫逃避相关的4种基因的检出率介于36.8%~68.4%:AdsA为42.1%(8/19)、chp为57.9%(11/19)、sbi为68.4%(13/19)、scn为36.8%(7/19)。葡萄球菌主要溶血毒素基因hlb和hld的检出率均为84.2%(16/19),而hla为63.2%(12/19)。SASCV中PVL(lukF/S)和lukD的检出率相对较低,均在40%以下,分别为26.3%(5/19)和36.8%(7/19)。
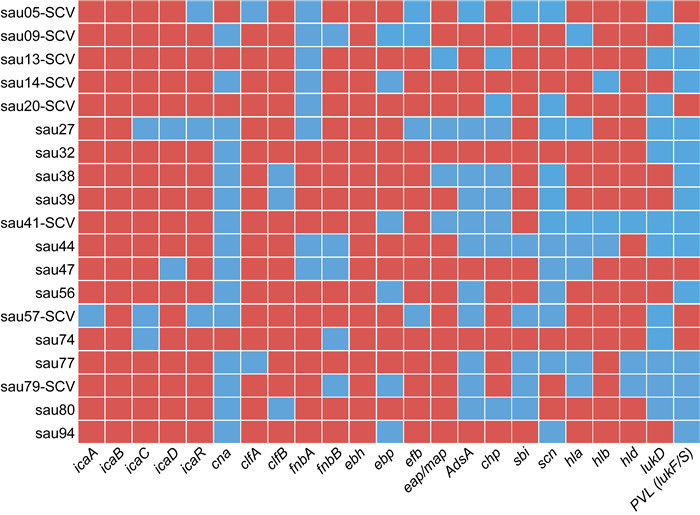
|
| Red means 'detected', and blue means 'not detected'. 图 3 19株SASCV中23种毒力基因检出情况 Fig. 3 Detection of 23 virulence genes in 19 SASCV strains |
全基因组序列与抗生素耐药基因数据库比对结果显示,19株SASCV耐药基因中blaZ检出率最高,为78.9%(15/19),mecA检出率为31.6%(6/19)。与红霉素、林可霉素及链霉素耐药相关的erm基因中,erm(B)检出率最高(31.6%,6/19),其次是erm(C)(15.8%,3/19)和erm(A)(10.5%,2/19)。其他耐药基因的检出率较低:与四环素耐药相关的tet基因中,tet(K)和tet(M)的检出率均为10.5%(2/19);与氨基糖苷类及甲氧苄啶耐药相关的基因中,aph(2″)-Ia(21.1%,4/19)、ant(6)-Ia(10.5%,2/19)、ant(9)-Ia(10.5%,2/19)、aph(3′)-III(10.5%,2/19)及dfrG(5.7%,1/19)均有检出。19株SASCV抗生素耐药基因检出情况具体如图 4所示。
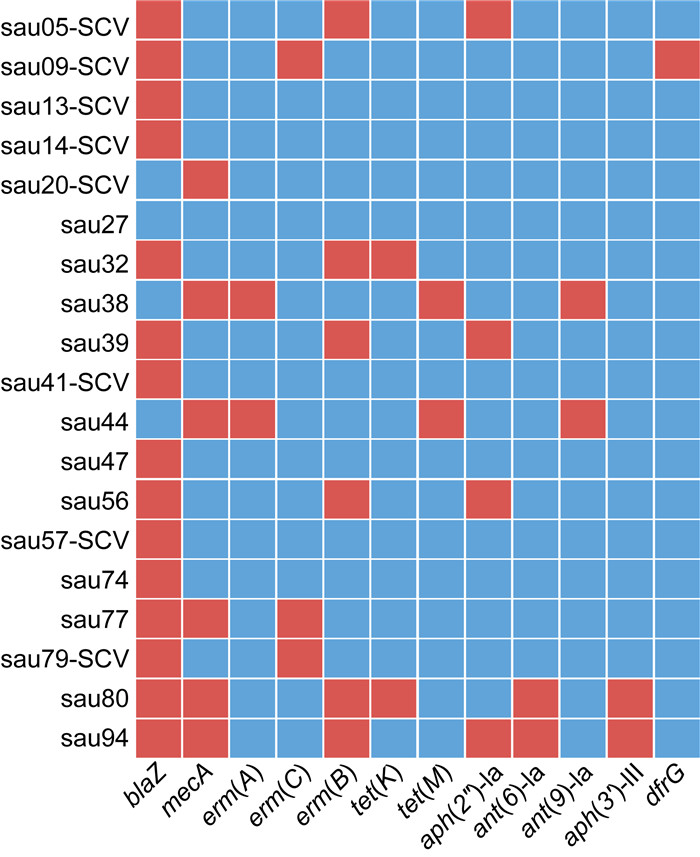
|
| Red means 'detected', and blue means 'not detected'. 图 4 19株SASCV中抗生素耐药基因检出情况 Fig. 4 Detection of antibiotic resistance genes in 19 SASCV strains |
PJI是人工关节置换术后的严重并发症之一,治疗失败率较高[3]。其主要病原菌是金黄色葡萄球菌,该菌也常引起皮肤软组织及其他外科术后感染。鉴于假体植入后关节组织内的特殊微环境,金黄色葡萄球菌可产生SASCV,表现为菌落变小,生长及代谢缓慢,可于细胞内寄生[16]。PJI中的SCV检出率高于其他感染类型。有文献报道98例晚期肺部疾病患者中SASCV感染率仅8%[17],而113例葡萄球菌所致PJI患者中SCV感染率为34%[18]。SASCV存在多种致病机制,与NP菌株相比其具有更强的侵入和定植骨组织的能力,可通过抑制趋化因子表达、胞内寄生及形成生物膜而逃避宿主免疫和抗生素的作用,导致其难以被清除[16]。Tande等[18]研究38例葡萄球菌SCV感染的PJI病例发现,与NP菌株感染者相比,葡萄球菌SCV感染持续时间更长,且与感染复发密切相关。因此,深入研究SASCV的毒力、耐药基因等分子特征,将有助于预防与控制此类感染。
金黄色葡萄球菌的致病力与其表达的多种黏附素有关,可通过细菌黏附和定植形成生物膜,而后者能够提供细菌生长繁殖的营养物质和酶类[19],同时增强细菌对抗生素的耐药性[20]和逃避宿主免疫细胞攻击的能力[9]。细胞间黏附基因簇icaADBC共同表达酶合成,并参与生物膜的形成,而icaR编码阻遏蛋白,调节icaADBC的表达[21-22]。本研究SASCV中的icaA、icaC、icaD、icaR基因的检出率很高(84.2%~94.7%),icaB检出率达100.0%(19/19)。Omidi等[23]在烧伤患者正常形态金黄色葡萄球菌感染中发现,icaA、icaD基因的检出率为77.6%。ebh编码的蛋白与纤维连接蛋白(fibronectin,fn)结合,参与细菌黏附聚集,与生物膜的形成密切相关[24-25]。魏莲花等[26]报道ebh在生物膜阳性组中的检出率为53.2%,而阴性组仅9.5%。本研究SASCV中ebh的检出率为100.0%,远高于既有研究的结果。此外,纤维连接蛋白结合蛋白a和b(FnbA和FnbB)以及凝集因子a和b(ClfA和ClfB)等黏附相关蛋白也是促进生物膜形成的重要因子[27-28]。本研究中,fnbA、fnbB、clfA、clfB的检出率依次为57.9%(11/19)、73.7%(14/19)、89.5%(17/19)、84.2%(16/19)。cna编码的蛋白可与胶原蛋白结合,介导金黄色葡萄球菌与结缔组织和软骨的黏附[29-30],在骨科植入物相关感染中具有重要作用[31-32]。在欧洲一项临床骨感染病原菌研究中,金黄色葡萄球菌中的cna流行率为38%~56%[29],本研究SASCV中cna检出率为21.1%(4/19)。以上结果提示,与金黄色葡萄球菌NP菌株相比,SCV中黏附素相关基因检出率较高。本研究还对金黄色葡萄球菌的毒力基因进行了分析,其中比较重要的是PVL。PVL由lukF-PV与lukS-PV两个基因编码,可在靶细胞膜上形成孔道,损伤细胞膜,从而促使白细胞凋亡、坏死[33]。本研究中PVL的检出率为26.3%。其他毒力基因还包括溶血毒素基因hla (63.2%)、hlb (84.2%)、hld (84.2%)以及免疫逃避相关基因AdsA (42.1%)、chp (57.9%)、sbi (68.4%)、scn (36.8%)。这些毒力因子参与SASCV黏附、侵袭及逃避宿主免疫,在致病机制中发挥了重要作用。
金黄色葡萄球菌的耐药问题早已引起广泛关注。本研究结果显示,SASCV中blaZ的检出率为78.9%(15/19),mecA的检出率为31.6%(6/19)。前者编码β -内酰胺酶,使青霉素水解而产生耐药;后者编码一种青霉素结合蛋白PBP2a,该蛋白与β -内酰胺类药物的亲和力降低,导致细菌对β -内酰胺类药物如青霉素类、头孢菌素类耐药,从而成为耐甲氧西林金黄色葡萄球菌(methicillin-resistant Staphylococcus aureus,MRSA)。文献报道的各地MRSA检出率不同,陕西髋关节PJI患者中MRSA的检出率为22.5%[34],成都为21.0%[35],本研究中为31.6%。MRSA还平均携带4~5个其他耐药基因,明显多于甲氧西林敏感金黄色葡萄球菌(methicillin-sensitive Staphylococcus aureus,MSSA),这是其多重耐药的原因[36],导致抗感染治疗难度提升,亟需临床医师的关注。erm编码核糖体甲基化酶,使23S rRNA甲基化,导致细菌对大环内酯类抗生素耐药,主要包括erm(A)、erm(B)、erm(C),金黄色葡萄球菌多以erm(A)、erm(C)为主,而本研究发现SASCV中erm(B)的检出率最高,其中原因须进一步研究。此外,SASCV中还检出氨基糖苷类抗生素耐药基因,如aph(2″)-Ia、ant(6)-Ia、ant(9)-Ia、aph(3′)-III,这是由于细菌获得并表达氨基糖苷类修饰酶基因或16S rRNA基因发生突变,导致该类药物失活。tet(K)、tet(M)编码核糖体保护蛋白或产四环素外排泵蛋白,从而导致细菌对四环素类耐药。
本研究中19株SCV和8株NP共分为10个ST,表明SASCV具有较高的遗传多样性,其中优势型别为ST59、ST398和ST25。既往成人及儿童骨科感染的金黄色葡萄球菌分子型别研究中,均以ST59为主[37-39],与本研究结果一致。亚太地区及我国文献报道中MRSA的优势型别以ST59为主[40-41],本研究结果与之相符,但欧洲研究发现MRSA主要型别为ST225、ST22[42],优势型别具有一定的地域差异,因此进一步研究SCV分子型别将有助于了解此类细菌亚群的流行病学特点。本研究对8组SCV和NP呈混合生长的样本进行全基因组测序与系统发育进化分析,结果显示2组(即sau41-SCV/sau41-NP和sau20-SCV/sau20-NP)的SCV与NP菌株在分子型别、菌种亲缘关系、毒力及耐药基因方面有较大差异,提示在日常微生物检验工作中决不可忽视SCV,应对NP和SCV菌株分别进行抗生素敏感试验,从而为临床提供准确的药敏报告。其余6组SCV与NP菌株的菌落形态虽不同,但其分子型别、毒力及耐药基因一致,可视为同一菌株。SASCV本身存在动态转变可能是造成此现象的原因之一。研究表明,部分SCV具有不稳定性、有营养缺陷、抗生素易感性等特点,可通过补偿性基因突变恢复到NP[43]。鉴于本研究中菌株数量较少,须增加样本量后进一步研究。
综上所述,本研究通过对SASCV进行全基因组测序及分析,发现SCV携带多种毒力及耐药基因,其中生物膜相关黏附素基因的检出率较高,耐药基因中mecA的检出率较高。分子型别中以ST59最多,其次为ST398和ST25。表型混合生长菌株中,SCV可与NP菌株分属不同型别,且携带的毒力及耐药基因差异较大。因此,须继续深入研究SASCV的分子病原学特征,从而有助于预防与控制此类感染。
| [1] |
Tsai Y, Chang CH, Lin YC, Lee SH, Hsieh PH, Chang Y. Different microbiological profiles between hip and knee prosthetic joint infections[J]. J Orthop Surg, 2019, 27(2): 2309499019847768.
[DOI]
|
| [2] |
Koh CK, Zeng I, Ravi S, Zhu M, Vince KG, Young SW. Periprosthetic joint infection is the main cause of failure for modern knee arthroplasty: an analysis of 11, 134 knees[J]. Clin Orthop Relat Res, 2017, 475(9): 2194-2201.
[DOI]
|
| [3] |
Bryan AJ, Abdel MP, Sanders TL, Fitzgerald SF, Hanssen AD, Berry DJ. Irrigation and debridement with component retention for acute infection after hip arthroplasty: improved results with contemporary management[J]. J Bone Joint Surg Am, 201, 99(23): 2011-2018.
[PubMed]
|
| [4] |
Lenguerrand E, Whitehouse MR, Beswick AD, Jones SA, Porter ML, Blom AW. Revision for prosthetic joint infection following hip arthroplasty: evidence from the National Joint Registry[J]. Bone Joint Res, 2017, 6(6): 391-398.
[DOI]
|
| [5] |
Nodzo SR, Boyle KK, Spiro S, Nocon AA, Miller AO, Westrich GH. Success rates, characteristics, and costs of articulating antibiotic spacers for total knee periprosthetic joint infection[J]. Knee, 2017, 24(5): 1175-1181.
[DOI]
|
| [6] |
Hischebeth GT, Randau TM, Ploeger MM, Friedrich MJ, Kaup E, Jacobs C, Molitor E, Hoerauf A, Gravius S, Wimmer MD. Staphylococcus aureus versus Staphylococcus epidermidis in periprosthetic joint infection—Outcome analysis of methicillin-resistant versus methicillin-susceptible strains[J]. Diagn Microbiol Infect Dis, 2019, 93(2): 125-130.
[DOI]
|
| [7] |
张少坤, 张珊珊, 刘永一, 许建中. 87例人工关节置换术后假体周围组织感染患者窦道分泌物标本细菌培养及耐药性分析[J]. 实验与检验医学, 2021, 39(3): 710-713. [DOI]
|
| [8] |
程翔, 梁玉龙, 邵宏翔, 宋洋, 郭宇. 假体周围感染病原菌及耐药性分析[J]. 中国矫形外科杂志, 2020, 28(11): 870-875. [CNKI]
|
| [9] |
Josse J, Valour F, Maali Y, Diot A, Batailler C, Ferry T, Laurent F. Interaction between staphylococcal biofilm and bone: how does the presence of biofilm promote prosthesis loosening?[J]. Front Microbiol, 2019, 10: 1602.
[DOI]
|
| [10] |
Nowicka J, Piątkowska E. Small colony variants—The cause of chronic infections[J]. Postep Mikrobiol (Adv Microbiol), 2021, 60(3): 183-194.
[DOI]
|
| [11] |
Liu J, Shen Z, Tang J, Huang Q, Jian Y, Liu Y, Wang Y, Ma X, Liu Q, He L, Li M. Extracellular DNA released by glycine-auxotrophic Staphylococcus epidermidis small colony variant facilitates catheter-related infections[J]. Commun Biol, 2021, 4(1): 904.
[DOI]
|
| [12] |
Masoud-Landgraf L, Zarfel G, Kaschnigg T, Friedl S, Feierl G, Wagner-Eibel U, Eber E, Grisold AJ, Kittinger C. Analysis and characterization of Staphylococcus aureus small colony variants isolated from cystic fibrosis patients in Austria[J]. Curr Microbiol, 2016, 72(5): 606-611.
[DOI]
|
| [13] |
Moldovan A, Fraunholz MJ. In or out: phagosomal escape of Staphylococcus aureus[J]. Cell Microbiol, 2019, 21(3): e12997.
[DOI]
|
| [14] |
Cai Y, Huang C, Chen X, Chen Y, Huang Z, Zhang C, Zhang W, Fang X. The role of Staphylococcus aureus small colony variants in intraosseous invasion and colonization in periprosthetic joint infection[J]. Bone Joint Res, 2022, 11(12): 843-853.
[DOI]
|
| [15] |
Fillingham YA, Della Valle CJ, Suleiman LI, Springer BD, Gehrke T, Bini SA, Segreti J, Chen AF, Goswami K, Tan TL, Shohat N, Diaz-Ledezma C, Schwartz AJ, Parvizi J. Definition of successful infection management and guidelines for reporting of outcomes after surgical treatment of periprosthetic joint infection: from the workgroup of the Musculoskeletal Infection Society (MSIS)[J]. J Bone Joint Surg Am, 2019, 101(14): e69.
[DOI]
|
| [16] |
Loss G, Simões PM, Valour F, Cortês MF, Gonzaga L, Bergot M, Trouillet-Assant S, Josse J, Diot A, Ricci E, Vasconcelos AT, Laurent F. Staphylococcus aureus small colony variants (SCVs): news from a chronic prosthetic joint infection[J]. Front Cell Infect Microbiol, 2019, 9: 363.
[DOI]
|
| [17] |
Kahl BC, Becker K, Löffler B. Clinical significance and pathogenesis of staphylococcal small colony variants in persistent infections[J]. Clin Microbiol Rev, 2016, 29(2): 401-427.
[DOI]
|
| [18] |
Tande AJ, Osmon DR, Greenwood-Quaintance KE, Mabry TM, Hanssen AD, Patel R. Clinical characteristics and outcomes of prosthetic joint infection caused by small colony variant staphylococci[J]. mBio, 2014, 5(5): e01910-14.
[DOI]
|
| [19] |
Achek R, Hotzel H, Nabi I, Kechida S, Mami D, Didouh N, Tomaso H, Neubauer H, Ehricht R, Monecke S, El-Adawy H. Phenotypic and molecular detection of biofilm formation in Staphylococcus aureus isolated from different sources in Algeria[J]. Pathogens, 2020, 9(2): 153.
[DOI]
|
| [20] |
Flemming HC, Wingender J, Szewzyk U, Steinberg P, Rice SA, Kjelleberg S. Biofilms: an emergent form of bacterial life[J]. Nat Rev Microbiol, 2016, 14(9): 563-575.
[DOI]
|
| [21] |
Lerch MF, Schoenfelder SMK, Marincola G, Wencker FDR, Eckart M, Förstner KU, Sharma CM, Thormann KM, Kucklick M, Engelmann S, Ziebuhr W. A non-coding RNA from the intercellular adhesion (ica) locus of Staphylococcus epidermidis controls polysaccharide intercellular adhesion (PIA)-mediated biofilm formation[J]. Mol Microbiol, 2019, 111(6): 1571-1591.
[DOI]
|
| [22] |
Fluckiger U, Ulrich M, Steinhuber A, Döring G, Mack D, Landmann R, Goerke C, Wolz C. Biofilm formation, icaADBC transcription, and polysaccharide intercellular adhesin synthesis by staphylococci in a device-related infection model[J]. Infect Immun, 2005, 73(3): 1811-1819.
[DOI]
|
| [23] |
Omidi M, Firoozeh F, Saffari M, Sedaghat H, Zibaei M, Khaledi A. Ability of biofilm production and molecular analysis of spa and ica genes among clinical isolates of methicillin-resistant Staphylococcus aureus[J]. BMC Res Notes, 2020, 13(1): 19.
[DOI]
|
| [24] |
Clarke SR, Harris LG, Richards RG, Foster SJ. Analysis of Ebh, a 1.1-megadalton cell wall-associated fibronectin-binding protein of Staphylococcus aureus[J]. Infect Immun, 2002, 70(12): 6680-6687.
[DOI]
|
| [25] |
Crosby HA, Tiwari N, Kwiecinski JM, Xu Z, Dykstra A, Jenul C, Fuentes EJ, Horswill AR. The Staphylococcus aureus ArlRS two-component system regulates virulence factor expression through MgrA[J]. Mol Microbiol, 2020, 113(1): 103-122.
[DOI]
|
| [26] |
魏莲花, 陈晓青, 李可可, 余甜, 谢跃, 王晓宁, 景双艳. 金黄色葡萄球菌生物膜形成及相关基因分析[J]. 临床检验杂志, 2019, 37(1): 38-40. [CNKI]
|
| [27] |
Soltani E, Farrokhi E, Zamanzad B, Shahini Shams Abadi M, Deris F, Soltani A, Gholipour A. Prevalence and distribution of adhesins and the expression of fibronectin-binding protein (FnbA and FnbB) among Staphylococcus aureus isolates from Shahrekord Hospitals[J]. BMC Res Notes, 2019, 12(1): 49.
[DOI]
|
| [28] |
Chen L, Tang ZY, Cui SY, Ma ZB, Deng H, Kong WL, Yang LW, Lin C, Xiong WG, Zeng ZL. Biofilm production ability, virulence and antimicrobial resistance genes in Staphylococcus aureus from various veterinary hospitals[J]. Pathogens, 2020, 9(4): 264.
[DOI]
|
| [29] |
Arciola CR, Visai L, Testoni F, Arciola S, Campoccia D, Speziale P, Montanaro L. Concise survey of Staphylococcus aureus virulence factors that promote adhesion and damage to peri-implant tissues[J]. Int J Artif Organs, 2011, 34(9): 771-780.
[DOI]
|
| [30] |
Puah SM, Tan JAMA, Chew CH, Chua KH. Diverse profiles of biofilm and adhesion genes in Staphylococcus aureus food strains isolated from sushi and sashimi[J]. J Food Sci, 2018, 83(9): 2337-2342.
[DOI]
|
| [31] |
Azmi K, Qrei W, Abdeen Z. Screening of genes encoding adhesion factors and biofilm production in methicillin resistant strains of Staphylococcus aureus isolated from Palestinian patients[J]. BMC Genomics, 2019, 20(1): 578.
[DOI]
|
| [32] |
Arciola CR, An YH, Campoccia D, Donati ME, Montanaro L. Etiology of implant orthopaedic infections: a survey on 1027 clinical isolates[J]. Int J Artif Organs, 2005, 28(11): 1091-1100.
[DOI]
|
| [33] |
Balakirski G, Hischebeth G, Altengarten J, Exner D, Bieber T, Dohmen J, Engelhart S. Recurrent mucocutaneous infections caused by PVL-positive Staphylococcus aureus strains: a challenge in clinical practice[J]. J Dtsch Dermatol Ges, 2020, 18(4): 315-322.
[DOI]
|
| [34] |
王瑛, 常军林. 髋关节置换术后假体周围感染的病原菌分布及耐药性分析[J]. 海南医学, 2022, 33(12): 1577-1579. [CNKI]
|
| [35] |
孙梦瑗, 汪璐, 曲远青, 王艳艳, 万娜. 成都地区骨科患者伤口金黄色葡萄球菌感染的分子流行病学及耐药性分析[J]. 暨南大学学报(自然科学与医学版), 2021, 42(1): 33-39. [DOI]
|
| [36] |
Wang S, Kang OH, Kwon DY. Bisdemethoxycurcumin reduces methicillin-resistant Staphylococcus aureus expression of virulence-related exoproteins and inhibits the biofilm formation[J]. Toxins (Basel), 2021, 13(11): 804.
[DOI]
|
| [37] |
王轶男, 凤梓涵, 徐磊, 姜北, 黎庶, 傅景曙, 谢肇, 王海连, 胡晓梅. 重庆西南医院骨科感染金黄色葡萄球菌的分子分型及耐药性研究[J]. 暨南大学学报(自然科学与医学版), 2016, 37(6): 481-487. [DOI]
|
| [38] |
Xu Z, Yuan C. Molecular epidemiology of Staphylococcus aureus in China reveals the key gene features involved in epidemic transmission and adaptive evolution[J]. Microbiol Spectr, 202, 10(5): e0156422.
[DOI]
|
| [39] |
Li J, Wang L, Ip M, Sun M, Sun J, Huang G, Wang C, Deng L, Zheng Y, Fu Z, Li C, Shang Y, Zhao C, Yu S, Yao K, Yang Y, Shen X. Molecular and clinical characteristics of clonal complex 59 methicillin-resistant Staphylococcus aureus infections in Mainland China[J]. PLoS One, 2013, 8(8): e70602.
[DOI]
|
| [40] |
Huh K, Chung DR. Changing epidemiology of community-associated methicillin-resistant Staphylococcus aureus in the Asia-Pacific region[J]. Expert Rev Anti Infect Ther, 2016, 14(11): 1007-1022.
[DOI]
|
| [41] |
隋新霞, 冯霞, 邵春红, 朱凯, 李栋, 胡军, 李心朋. 血流感染金黄色葡萄球菌分子生物学特征[J]. 中华医院感染学杂志, 2022, 32(10): 1459-1463. [CNKI]
|
| [42] |
Grundmann H, Schouls LM, Aanensen DM, Pluister GN, Tami A, Chlebowicz M, Glasner C, Sabat AJ, Weist K, Heuer O, Friedrich AW, ESCMID Study Group on Molecular Epidemiological Markers, European Staphylococcal Reference Laboratory Working Group. The dynamic changes of dominant clones of Staphylococcus aureus causing bloodstream infections in the European region: results of a second structured survey[J]. Euro Surveill, 2014, 19(49): 20987.
[DOI]
|
| [43] |
Melter O, Radojevič B. Small colony variants of Staphylococcus aureus—review[J]. Folia Microbiol (Praha), 2010, 55(6): 548-558.
[DOI]
|
 2023, Vol. 18
2023, Vol. 18


